Whether you’re a small independent practice or a large, complex healthcare organization, our experienced professionals can optimize your cash flow.

Enter patient and insurance eligibility.

Verify insurance coverage and pre-authorizations.

Collect payments and update patient details.

Assign medical codes accurately.

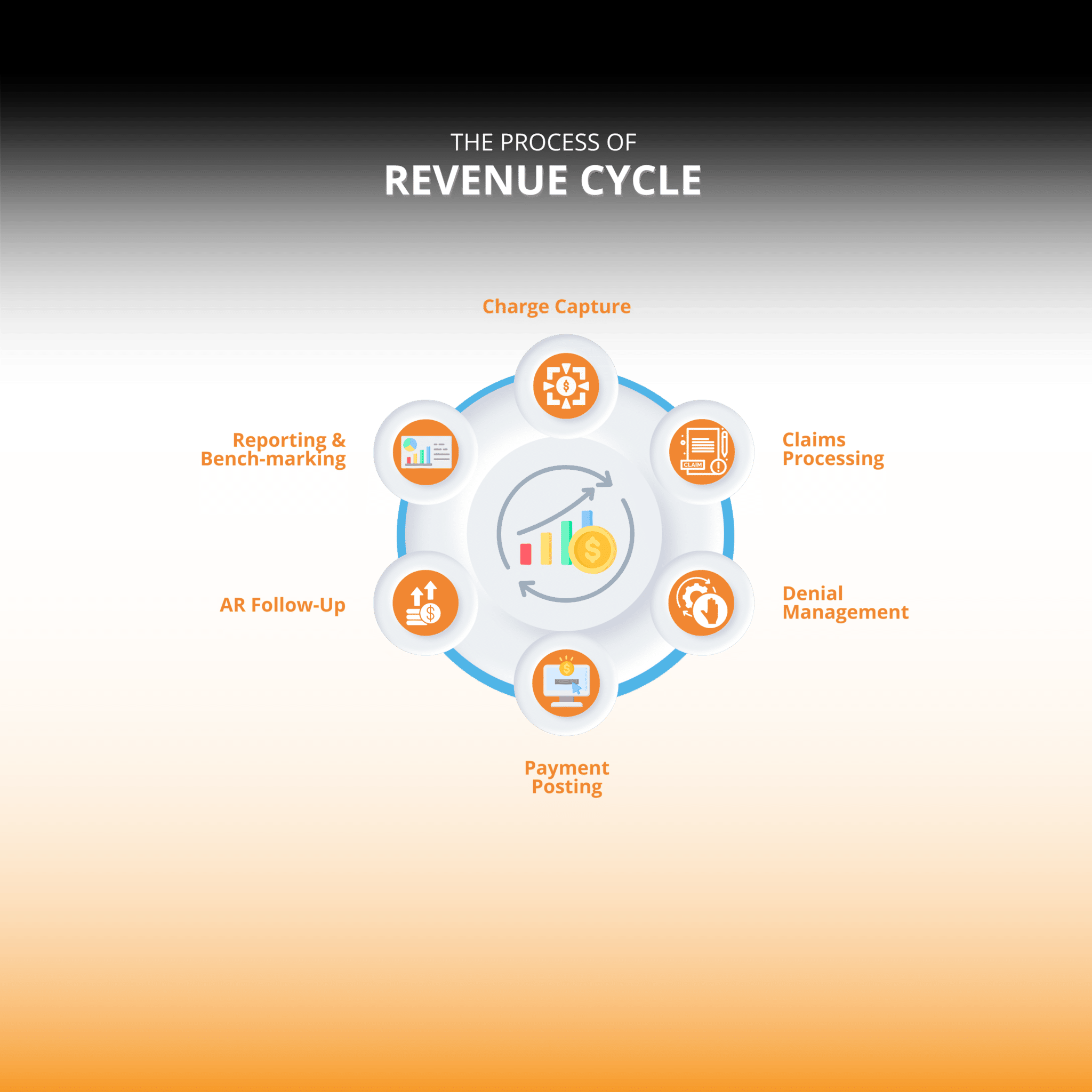
Enter service charges into the system.

Submit claims to insurance companies.

Insurance review, adjudication, and payment determination.

Record payments from insurance and patients.

Monitor and address unpaid or underpaid claims.

Send statements and assist with billing inquiries.

Reconcile payments with expected revenue.

Analyze, appeal, and reduce claim denials.

Generate and analyze performance reports.

Follow up on outstanding balances and set up payment plans.

Close accounts after receiving and processing all payments.